This is where it all started, I was locked outside Friend's house waiting for her to return for our group study session for which I was the only one remotely on time. I decided I'd start studying anyway, despite the fact it was cold like the grave. As you've probably quickly noticed, I enjoy playing with words and anti-thrombin III just rearranged itself in my head into Aunty From Bin III, and by the time Friend arrived and let me in I was madly scribbling pictures as fast as I could.

Anti-thrombin III is the main agent against clotting.

Heparin interacts with Anti-thrombin III and inhibits factors 9-12a and thrombin II

Thrombin II cleaves fibrinogen into fibrins and also aggregates platelets, stimulates cell proliferation and modulates smooth muscle contraction
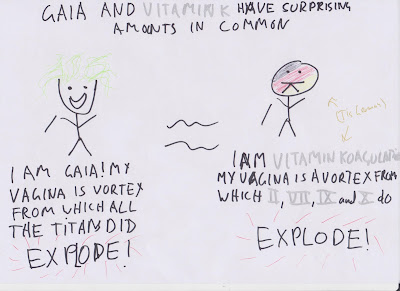
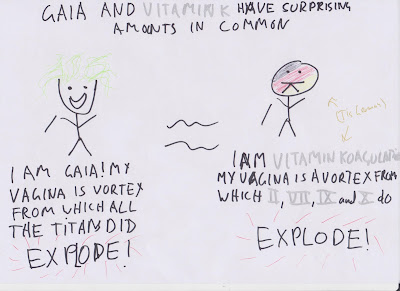
Vitamin K makes factors 2,7,9 and 10. The common F2A channels in Australia.
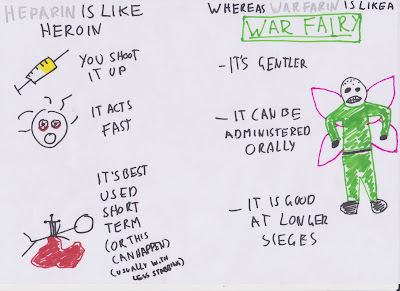
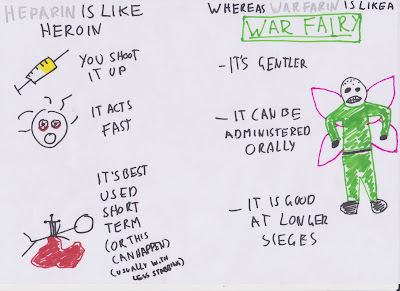
Heparin -IV, fast, short term. Warfarin - Oral, slower, longer term
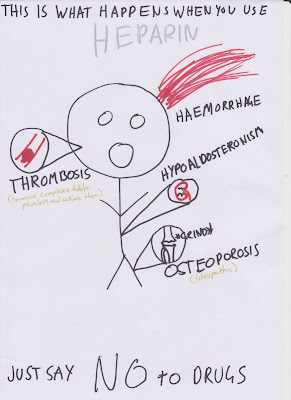
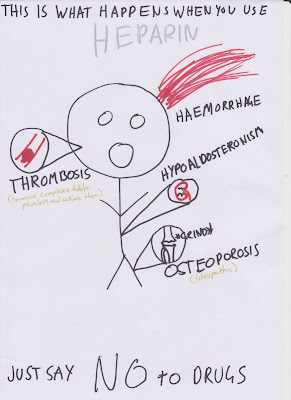
Heparin can cause haemorrhage, thrombosis (oddly), hypoaldosteronism and osteoporosis
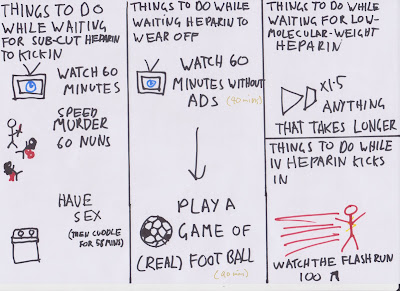
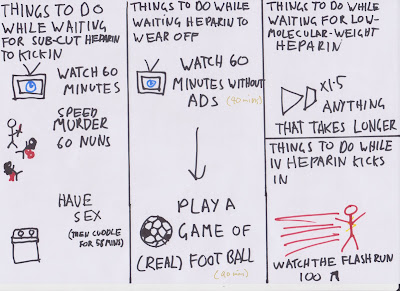
Heparin IV onset is almost immediate, with s/c it takes about an hour, and it takes 40-90 minutes to wear off. Low Molecular Weight heparin takes longer.
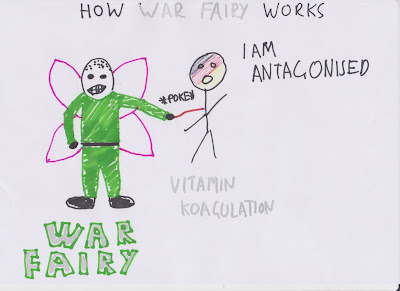
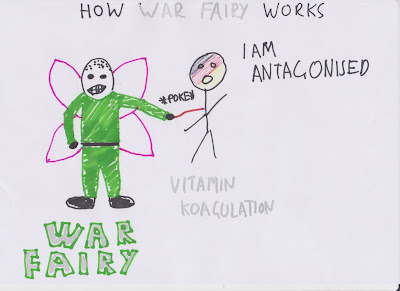
Warfarin is a Vitamin K antagonist

Warfarin is absorbed by the gut, and therefore administered orally, is teratogenic, can occasionally be hepatotoxic, can cause haemorrhage and have a narrow therapeutic window.

I don't really understand this, but those are the basic principles.
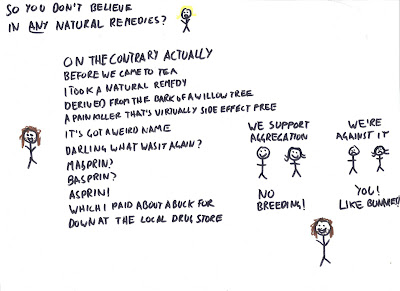
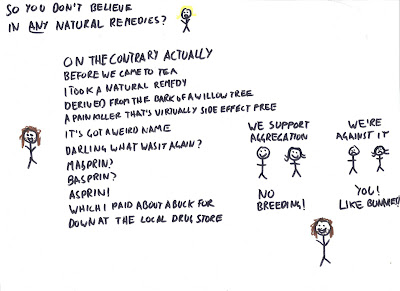
Asprin inhibits production of TXA2 which promotes aggregation and promotes production of PCI2 which inhibits platelet aggregation.

Dipyridamole is a phosphodiesterase inhibitor, but just remember it's an anti-platelet drug.
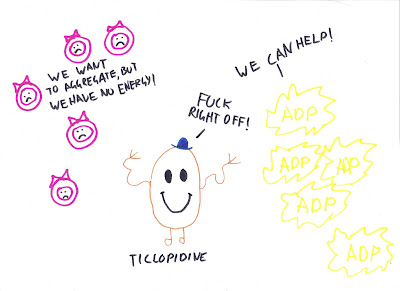
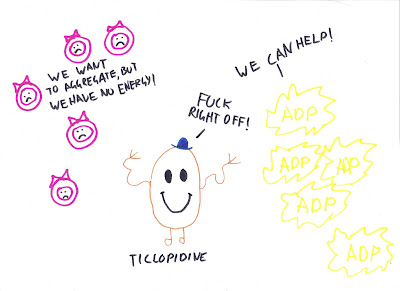
Thienopyridine derivatives (Ticlopidine and clopidogrel) inhibit ADP-dependent aggregation

Seriously. Abciximab? Who the hell came up with that name? Were they trying to summon Cthulhu?

But ridiculous name aside, abciximab, along with tirofiban and eptifibatide, are often given as adjuncts to heparin and aspirin, to reduce restenosis. All of these are glycoprotein IIB/IIIA receptor antagonists.
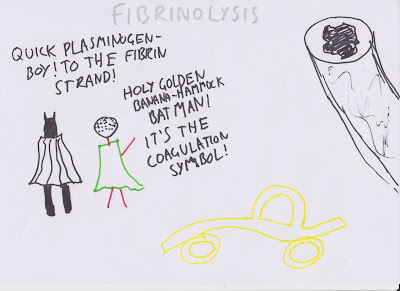
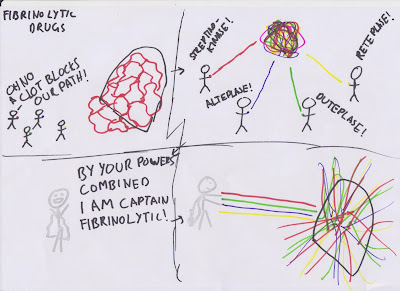
The fibrinolytic system is activated at the same time as the coagulation system, and plasminogen is deposited on fibrin strands.
Streptinokinase, alteplase, duteplase and reteplase are fibrinolytic drugs with slightly different mechanisms, but in practise they have all been shown to have equal long term outcomes.